Cancer has a biological clock and this drug may keep it from ticking
A new drug shows potential to halt cancer cells’ growth by stunting the cells’ biological clock.
The findings from scientists at the USC Michelson Center for Convergent Bioscience and Nagoya University’s Institute of Transformative BioMolecules (ITbM) advance a burgeoning area of research: turning the body’s circadian rhythms against cancer.
Their study, conducted on human kidney cancer cells and on acute myeloid leukemia in mice, was published Jan. 23 in the journal Science Advances.
Scientists know that disrupting sleep and other elements of humans’ circadian rhythm can harm health. The same is true for the circadian clock of cells themselves. If researchers could disturb the circadian clock of cancer cells, they theorize, they could potentially hurt or kill those cells.
The scientists found that a molecule named GO289 targets an enzyme that controls the cell’s circadian rhythm. This drug-protein interaction then disrupts the functions of four other proteins that are important for cell growth and survival.
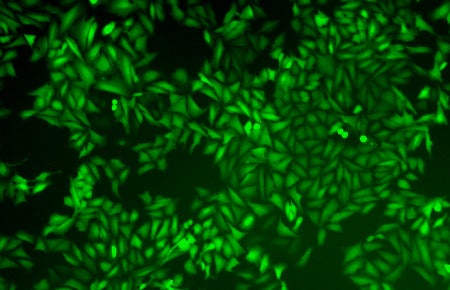
Human bone cancer cells stopped growing when a drug molecule jammed their circadian rhythm during a study that appears in Science Advances. (Image: Courtesy of the Kay lab at the USC Michelson Center for Convergent Bioscience.)
In effect, GO289 can jam the cogs of the cell’s circadian clock, slowing its cycles. And it can do so with little impact to healthy cells.
“In some cancers, the disease takes over the circadian clock mechanism and uses it for the evil purpose of helping itself grow,” said Steve Kay, director of convergent biosciences at the USC Michelson Center and Provost Professor of Neurology, Biomedical Engineering and Biological Sciences. “With GO289, we can interfere with those processes and stop the cancer from growing.”
Kay is among several scientists from USC Dornsife College of Letters, Arts and Sciences, USC Viterbi School of Engineering and Keck School of Medicine of USC who are collaborating across multiple disciplines to find new solutions for treating cancer, neurological disease and cardiovascular disease.
Finding the right candidate
On its initial interactions with human bone cancer cells, GO289 appeared to slow the tumors’ circadian clock as it targeted an enzyme, named CK2.
To see if GO289 consistently hindered other cancers in the same way, the scientists then tested it on human kidney cancer cells and on mice with acute myeloid leukemia. They found that GO289 specifically affected cancer cell metabolism and other circadian-related functions that normally would enable the cancer to grow and spread.
Kay is optimistic about the findings. “This could become an effective new weapon that kills cancer,” he said.
About the study
In addition to Kay and Hirota, other study co-authors were ITBM researchers Tsuyoshi Oshima, Yoshimi Niwa, Keiko Kuwata, Ashutosh Srivastava, Tomoko Hyoda, as well as Yoshiki Tsuchiya of Kyoto Prefectural University of Medicine , Megumi Kumagai of Seitama Medical University, Masato Tsuyuguchi of Osaka Prefecture University, and Teruya Tamaru of Toho University School of Medicine, Akiko Sugiyama of ITBM, Natsuko Ono, Norjin Zolboot, Yoshiki Aikawa, Shunsuke Oishi as well as Atushi Nonami of Kyushu University Graduate School of Medical Sciences, Fumio Aria of Kyushu University, Shinya Hagihara of ITBM, Junichiro Yamaguchi of Waseda University, Florence Tama of ITBM, Yuya Kunisaki of Kyushu University Graduate School of Medical Sciences, Kazuhiro Yagita of Kyoto Prefectural University of Medicine, Masaaki Ikeda of Saitama Medical University, Takayoshi Kinoshita of Osaka Prefecture University, and Kenichiro Itami of ITBM.
Funding sources for the work include PRESTO Grant JPMJPR14LA from JST AQ49AQ50 (to T.Hi.); Grant-in-Aid for Research Activity start-up 26891011, Young Scientists (A) 15H05590, and Scientific Research (B) 18H02402 from JSPS (to T.Hi.); the Naito Foundation (to T.Hi.); the
Inamori Foundation (to T.Hi.); the Takeda Science Foundation (to T.Hi.); Grant-in-Aid for JSPS
Fellows 16J04435 (to T.O.) and 15J05509 (to Y.N.) from JSPS; Grant-in-Aid for Scientific AQ51 Research (B) 18H02841 from JSPS (to Y.K.); and Grant-in-Aid for Scientific Research 26119006
and 15K21711 from JSPS (to F.T.). Preliminary experiments and diffraction data collection werecarried out at the beamline BL17A of the Photon Factory (proposal no. 2016G665) and at the Osaka University beamline BL44XU of SPring-8 (proposal no. 2015A6518).