Fasting and Radiation Therapy
A new study from USC Dornsife researchers is the first to show that controlled fasting improves the effectiveness of radiation therapy in cancer treatments, extending life expectancy in mice with aggressive brain tumors.
Prior work by Valter Longo, professor of gerontology and biological sciences in USC Dornsife, corresponding author on the study and director of the Longevity Institute at the USC Davis School of Gerontology, has shown that short-term fasting protects healthy cells while leaving cancer cells vulnerable to the toxic effects of chemotherapy.
The latest study published online in PLOS One, is the first to show that periods of fasting appear to have the same augmenting effect on radiation therapy in treating gliomas, the most commonly diagnosed brain tumor. Patients with high-grade gliomas have a median survival rate of less than two years.
“With our initial research on chemotherapy, we looked at how to protect patients against toxicity,” Longo said. “With this research on radiation, we’re asking, what are the conditions that make cancer most susceptible to treatment? How can we replicate the conditions that are least hospitable to cancer?”
Longo and his co-investigators, which included Thomas Chen, co-director of the Neuro-Oncology program at the USC/Norris Cancer Center, studied the combination of fasting with radiation therapy and with the chemotherapy drug Temozolomide, currently the standard agent used for the treatment of brain tumors in adults after an attempt at surgical removal.
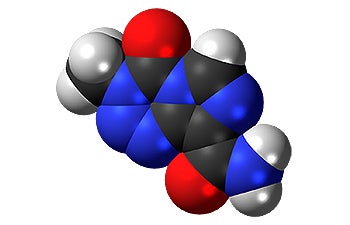
A model of the chemotherapy drug Temozolomide, currently the standard agent used to treat gliomas in adults.
The researchers found that controlled short-term fasting in mice, no more than 48 hours each cycle, improved the effectiveness of radiation and chemotherapy in treating gliomas. Despite the extremely aggressive growth of the type of brain tumor studied, more than twice as many mice that fasted and received radiation therapy survived to the end of the trial period than survived with radiation alone or fasting alone.
“The results demonstrate the beneficial role of fasting in gliomas and their treatment with standard chemotherapy and radiotherapy,” the researchers wrote. They said the results indicated the benefits of short-term, controlled fasting for humans receiving treatment for brain tumors.
Longo cautioned that patients should consult with their oncologist before undertaking any fasting: “You want to balance the risks. You have to do it right. But if the conditions are such that you’ve run out of options, short-term fasting may represent an important possibility for patients.”
The USC Norris Comprehensive Cancer Center, Mayo Clinic and Leiden University Hospital are all conducting clinical trials on fasting and chemotherapy. A clinical trial on glioma, fasting and radiotherapy is also being considered at USC.
Fernando Safdie of the USC Andrus Gerontology Center and Sebastian Brandhorst of Centre for Medical Biotechnology, Germany, were co-lead authors of the study. Min Wei, Changhan Lee and Saewon Hwang of the USC Andrus Gerontology Center; Weijun Wang and Chen of the USC Norris Neuro-oncology program at the Keck School of Medicine of USC; and Peter Conti of the Molecular Imaging Center at the Keck School were co-authors.
The research was funded by the National Institutes of Aging in the National Institute of Health, the Bakewell Foundation, The V Foundation for Cancer Research and a USC Norris Cancer Center pilot grant.